Endometrium
| Endometrium | |
|---|---|
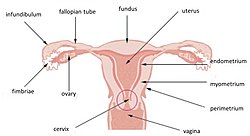 | |
| Uterus and uterine tubes. (Endometrium labeled at center right.) | |
| Latin | tunica mucosa uteri |
| Gray's | subject #268 1262 |
| MeSH | Endometrium |
| Dorlands/Elsevier | Endometrium |
The endometrium is the inner membrane of the mammalian uterus.
Function
The endometrium functions as a lining for the uterus, preventing adhesions between the opposed walls of the myometrium, thereby maintaining the of the uterine cavity. During the menstrual cycle or estrous cycle, the endometrium grows to a thick, blood vessel-rich, glandular tissue layer. This represents an optimal environment for the implantation of a blastocyst upon its arrival in the uterus. The endometrium is central, echogenic (detectable using ultrasound scanners), and has an average thickness of 6.7mm.
During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and foetus.
Cycle
The endometrial lining undergoes cyclic regeneration. Humans and the great apes display the menstrual cycle, whereas most other mammals are subject to an estrous cycle. In both cases, the endometrium initially proliferates under the influence of estrogen. However, once ovulation occurs, in addition to estrogen, the ovary will also start to produce progesterone. This changes the proliferative pattern of the endometrium to a secretory lining. Eventually, the secretory lining provides a hospitable environment for one or more blastocysts. If a blastocyst implants, then the lining remains as decidua. The decidua becomes part of the placenta; it provides support and protection for the gestation.
If there is inadequate stimulation of the lining, due to lack of hormones, the endometrium remains thin and inactive. In humans, this will result in amenorrhea. After menopause, the lining is often described as being atrophic. In contrast, endometrium that is chronically exposed to estrogens, but not to progesterone, may become hyperplastic.
In humans, the cycle of building and shedding the endometrial lining lasts an average of 28 days. The endometrium develops at different rates in different mammals. Its formation is sometimes affected by seasons, climate, stress, and other factors. The endometrium itself produces certain hormones at different points along the cycle. This affects other portions of the reproductive system.
Histology
The endometrium consists of a single layer of columnar epithelium, resting on a layer of connective tissue, which varies in thickness according to hormonal influences - the stroma. Simple tubular uterine glands reach from the endometrial surface through to the base of the stroma, which also carries a rich blood supply of spiral arteries. In a woman of reproductive age, two layers of endometrium can be distinguished. These two layers occur only in endometrium lining the cavity of the uterus, not in the lining of the Fallopian tubes:
In the absence of progesterone, the arteries supplying blood to the functional layer constrict, so that cells in that layer become ischaemic and die, leading to menstruation.
It is possible to identify the phase of the menstrual cycle by observing histological differences at each phase:
Pathological conditions
Adenomyosis is the growth of the endometrium into the muscle layer of the uterus (the myometrium).
Endometriosis is the growth of endometrial tissue outside the uterus.
Endometrial cancer is the most common cancer of the human female genital tract.
Asherman's syndrome, also known as intrauterine adhesions occurs when the basal layer of the endometrium is damaged by instrumention (e.g. D&C) or infection (e.g. endometrial tuberculosis) resulting in endometrial sclerosis and adhesion formation partially or completely obliterating the uterine cavity.
Thin endometrium may be defined as an endometrial thickness of less than 8 mm. It usually occurs after menopause. Treatments that can improve endometrial thickness include Vitamin E, L-arginine and sildenafil citrate.
Gene expression profiling using cDNA microarray can be used for the diagnosis of endometrial disorders.
See also
Additional images
References
- Blue Histology - Female Reproductive System. School of Anatomy and Human Biology - The University of Western Australia http://www.lab.anhb.uwa.edu.au/mb140/CorePages/FemaleRepro/FemaleRepro.htm Accessed 20061228 20:35
- Takasaki A, Tamura H, Miwa I, Taketani T, Shimamura K, Sugino N (April 2010). "Endometrial growth and uterine blood flow: a pilot study for improving endometrial thickness in the patients with a thin endometrium". Fertil. Steril. 93 (6): 1851–8. doi:10.1016/j.fertnstert.2008.12.062. PMID 19200982.
- Tseng, L.; Chen, I.; Chen, M.; Yan, H.; Wang, C.; Lee, C. (2010). "Genome-based expression profiling as a single standardized microarray platform for the diagnosis of endometrial disorder: an array of 126-gene model". Fertility and sterility 94 (1): 114–119. doi:10.1016/j.fertnstert.2009.01.130. PMID 19328470.
External links
- SUNY Figs 43:05-15 - "The uterus, uterine tubes and ovary with associated structures."
- Histology at BU 18902loa - "Female Reproductive System uterus, endometrium"
- Swiss embryology (from UL, UB, and UF) gnidation/role02
- Histology at OU 20_01
- Histology at utah.edu. Slide is proliferative phase - click forward to see secretory phase
Retrieved from : http://en.wikipedia.org/wiki/Endometrium
No comments:
Post a Comment